 A new study confirms health benefits of moderate calorie restriction in people and identified a key protein that might be utilized to extend human health. Previous research has shown that restricting calorie intake by worms, mice and flies can enhance the span of life in lab conditions. However, whether calorie restriction is able to do the same for humans has remained unclear.
A new study confirms health benefits of moderate calorie restriction in people and identified a key protein that might be utilized to extend human health. Previous research has shown that restricting calorie intake by worms, mice and flies can enhance the span of life in lab conditions. However, whether calorie restriction is able to do the same for humans has remained unclear.
This was the first controlled study of restricting calories in healthy humans and the research was based on the clinical study CALERIE (Comprehensive Assessment of Long Term Effects of Reducing Intake of Energy).
The researchers first created a baseline of calories consumed for over 200 participants. They asked a portion of the participants to reduce calories by 14% while the remaining participants continued to eat as normal. The long term effects to their health were analyzed for 2 years.
The main intent of the clinical trial was to observe if restricting calories is as beneficial to humans as it is for animals in the lab. They wanted to understand what restricting calories does to the human body and, specifically if it can lead to improved health. Previous research on mice had shown restricting calories can increase infections. So the team wanted to see how restricting calories might have a link to inflammation and the response of the immune system.
In humans chronic low grade inflammation is a significant trigger of a variety of chronic diseases, therefore having an adverse effect on life span. They wanted to answer what does restricting calories do to the metabolic and immune systems. If it is beneficial, then how do we control the endogenous pathways that copy its effects in humans?
The team began by analyzing the thymus gland which is located above the heart and produces T cells. T cells are a crucial part of our immune system as they are a type of white blood cell. This gland will age faster than other organs, and as it ages it produces fewer T cells. When healthy adults are around 40 years old, 70% of this gland is already nonfunctional and fatty. As we age, we begin to feel the absence of brand new T cells as the ones we have left are not good at fighting new pathogens. This is one of the reasons older people are at a greater risk for illnesses.
The team used MRI to determine if there were beneficial differences between the thymus glands of the participants on the restricted calorie diet and those who were not. They discovered that the gland in the participants on the restricted calorie diet had greater function volume and less fat after 2 years of restricting their calories. This meant they were producing more T cells than they did at the beginning of the study. The participants who were not calorie restricted did not show any change in functional volume.
The team was amazed that the thymus gland can be rejuvenated noting that there is hardly any evidence of it occurring in humans. This dynamic effect on this gland had the team expecting to also discover changes to the immune cells that the gland was producing. If so, then there could be underlying overall benefits of restricting calories. However, when they sequenced the genes in these cells, they discovered there were not any changes in gene expression after the two year period.
This observation had the team look closer which showed a surprising discovery – it turned out the action was really in the tissue miscroenvironment and not the blood T cells.
The team had studied adipose tissue which is body fat of the participants on the calorie restricted diet at three different points – the beginning, at one year and at the 2 year end of the study. Body fat is essential as it delivers a strong immune system. The are a variety of immune cells that occur in fat and when they are atypically activated they turn into a source of inflammation.
The team discovered amazing changes in the gene expression of adipose tissue at one year that were sustained to two years. This showed some genes were involved in the extension of life in animals and also unique restriction mimicking of calorie targets that could improve anti-inflammatory and metabolic responses in people.
The team then set out to observe if any genes they had identified in the analysis could be driving some of the benefits of restricting calories. They looked at the gene for PLA2G7 which is one of the genes that was significantly inhibited after restricting calories. PLA2G7 is a protein that is produced by immune cells that are known as macrophages.
The change in PLA2G7 gene expression that was observed in the participants who limited their calories suggested the protein could be linked to the effects of restricting calories. The team also tracked what would happen when the protein was reduced in mice in a lab.
They discovered that reducing the protein in mice yielded similar benefits that were seen in the participants on the calorie restricted diet. The thymus gland of the mice was functional for a longer period. They were protected from weight gain due to diet and were also protected from inflammation due to the aging process.
The effects occurred due to PLA2G7 targeting a specific mechanism of inflammation known as NLRP3. Lowering PLA2G7 protected the older mice from inflammation.
The findings show that PLA2G7 is a driver of the effects of restricting calories. The identification of these drivers helps the team determine how the immune system and the metabolic system speak to each other. This can point to potential targets which can improve function of the immune system and reduce inflammation and possibly enhance a healthy lifespan.
For example, it could be possible to manipulate PLA2G7 and receive the benefits of restricting calories without having to actuall restrict calories which can be harmful for some humans.
CALERIE is a controlled study that indicated that a simple restriction of calories with no specific diet, has a significant effect of shifting the immuno-metabolic state in a direction that protects human health. It gives great hope.
To view the original scientific study click below:
Caloric restriction in humans reveals immunometabolic regulators of health span
Caloric restriction has a new player
 The team investigated the connection between cancer risk and diet through analyzing data from 472,377 British adults from the UK Biobank during the years 2006-2010. The participants were 40-70 years old and reported they consumed fish and meat. Using health records, the research team calculated the occurrence of cancers that had developed roughly over 11 years. They took into account sociodemographics, diabetes status, socioeconomics and other lifestyle factors.
The team investigated the connection between cancer risk and diet through analyzing data from 472,377 British adults from the UK Biobank during the years 2006-2010. The participants were 40-70 years old and reported they consumed fish and meat. Using health records, the research team calculated the occurrence of cancers that had developed roughly over 11 years. They took into account sociodemographics, diabetes status, socioeconomics and other lifestyle factors. 


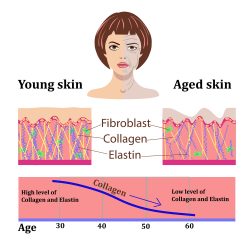 Scientists from the Babraham Institute in Cambridge have discovered a new technique to rejuvenate old skin cells. This technique has the ability for researchers to turn back time for up to 30 years on cellular aging without changing their function.
Scientists from the Babraham Institute in Cambridge have discovered a new technique to rejuvenate old skin cells. This technique has the ability for researchers to turn back time for up to 30 years on cellular aging without changing their function.  A new study confirms health benefits of moderate calorie restriction in people and identified a key protein that might be utilized to extend human health. Previous research has shown that restricting calorie intake by worms, mice and flies can enhance the span of life in lab conditions. However, whether calorie restriction is able to do the same for humans has remained unclear.
A new study confirms health benefits of moderate calorie restriction in people and identified a key protein that might be utilized to extend human health. Previous research has shown that restricting calorie intake by worms, mice and flies can enhance the span of life in lab conditions. However, whether calorie restriction is able to do the same for humans has remained unclear.  A new study has discovered a way to regrow or replace bone that has been lost by using high frequency sound waves. Researchers from RMIT University showed how this could be done faster and more efficiently than any process now in use.
A new study has discovered a way to regrow or replace bone that has been lost by using high frequency sound waves. Researchers from RMIT University showed how this could be done faster and more efficiently than any process now in use. 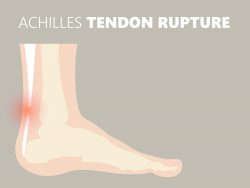 Tendons are the structures that connect our muscles to our bones. They are important to every movement a person does. When they become injured, it can be quite difficult to repair them. The existing therapies often are fret with complications. In a quest to remedy this, researchers have now constructed artificial tendons. They are biologically and mechanically similar to normal tendons and use human pluripotent stem cells.
Tendons are the structures that connect our muscles to our bones. They are important to every movement a person does. When they become injured, it can be quite difficult to repair them. The existing therapies often are fret with complications. In a quest to remedy this, researchers have now constructed artificial tendons. They are biologically and mechanically similar to normal tendons and use human pluripotent stem cells.  There are actions all of us can take in an effort to boost our odds for a long life. Some of these are staying active, getting plenty of sunlight, having a sleep rountine, eating healthy and keeping up a good mood.
There are actions all of us can take in an effort to boost our odds for a long life. Some of these are staying active, getting plenty of sunlight, having a sleep rountine, eating healthy and keeping up a good mood. Age is not only a number, but a variety of things that carry unwanted side effects such as weaker muscles, brittle bones, and risks for cancer and cardiovascular disease. Scientists have now shown they can effectively and safely reverse the process of aging in elderly and middle aged mice by partly resetting their cells to more youthful conditions.
Age is not only a number, but a variety of things that carry unwanted side effects such as weaker muscles, brittle bones, and risks for cancer and cardiovascular disease. Scientists have now shown they can effectively and safely reverse the process of aging in elderly and middle aged mice by partly resetting their cells to more youthful conditions. New research from Boston has shown success in the regrowth of human corneal tissue from adult stem cells to restore vision. Whether corneal tissue loss is due to damage from burns, chemical injury or eye diseases it is one of the leading reasons for blindness. This new groundbreaking process has the potential to restore vision in people that are blind.
New research from Boston has shown success in the regrowth of human corneal tissue from adult stem cells to restore vision. Whether corneal tissue loss is due to damage from burns, chemical injury or eye diseases it is one of the leading reasons for blindness. This new groundbreaking process has the potential to restore vision in people that are blind. As you think about what to drink and eat to help with aging, have you ever wondered what is the best fruit for anti-aging?
As you think about what to drink and eat to help with aging, have you ever wondered what is the best fruit for anti-aging? A recent study has shown that people with a high degree of body fat are at risk for a reduction in their cognitive function. Even when vascular brain injuries or cardiovascular risks were taken into consideration, the link associated with body fat and cognitive scores being lower remained the same. This has suggested that not yet confirmed pathways link cognitive function reduction and excess body fat.
A recent study has shown that people with a high degree of body fat are at risk for a reduction in their cognitive function. Even when vascular brain injuries or cardiovascular risks were taken into consideration, the link associated with body fat and cognitive scores being lower remained the same. This has suggested that not yet confirmed pathways link cognitive function reduction and excess body fat.