Immune Aging Accelerated By Stress
 A new study demonstrates that stress from things like job strain, traumatic events, discrimination, and everyday occurrences can accelerate immune system aging. This can possibly increase people’s chances of cardiovascular disease, cancer and illness due to infections. The study could offer an explanation in disparities in health that are age related which include the diverse toll of the COVID-19 pandemic and determine possible avenues for intervention.
A new study demonstrates that stress from things like job strain, traumatic events, discrimination, and everyday occurrences can accelerate immune system aging. This can possibly increase people’s chances of cardiovascular disease, cancer and illness due to infections. The study could offer an explanation in disparities in health that are age related which include the diverse toll of the COVID-19 pandemic and determine possible avenues for intervention.
Because the worldwide population of aging people is increasing, the understanding of disparities in health that are age related is essential. The study helps to identify mechanisms connected to immune aging that is accelerated.
As we age, our immune system will naturally start a dramatic downturn which is a condition known as immunosenescence. As advanced age occurs, a person’s immune system will weaken and include many white blood cells that are not circulating and not enough that are naive and can take on new invaders.
The aging of the immune system is linked not only to cancer, but also with a heightened risk of cardiovascular disease, pneumonia, and reduced efficacy of aging organs.
The team wanted to see if they might be able to coax out a link between a life long exposure to stress, which is a known precursor to health that is poor, and declining intensity of the immune system.
They cross referenced and queried an enormous amount of data sets from the Univ. of Michigan and Retirement Study, which was a national study of the status of health, economic, marital and family position, and private and public support systems of Americans that were older.
To determine exposure to a variety of social stressors, the team studied answers from a national sampling of 5,744 individuals over age 50. A questionnaire was designed for the participants to answer that assessed respondents experiences with social stress that included chronic stress, life events that are stressful, ongoing discrimination and everyday discrimination.
Samples of blood from the participants were then analyzed through flow cytometry, a lab technique that classifies and counts blood cells as they flow one by one in a narrow stream by a laser.
As was expected, participants with a high stress score had older immune profiles with a lower percentage of disease fighters and a high percentage of white blood cells that were worn out. The association between stressful life events and fewer, ready to respond T cells, continued to be strong even following controlling of smoking, education, BMI, race, drinking and ethnicity.
T cells are critical components of immunity develop in the thymus gland, which is in front and above the heart. As we age, the tissue in the thymus gland diminshes and is replaced by fatty tissue which results in decreased production of immune cells. Earlier research has suggested that this process is sped up by lifestyle factors like low exercise, poor diet, which are both linked with social stress.
In the study, after the team statistically controlled for low exercise and poor diet, the association between stress and increased immune aging wasn’t as strong. This means people who go through more stress have poor exercise and diet habits, which partly explains why they have increased aging. Improving exercise and diet habits in older people might help counteract the immune aging linked with stress.
Also, CMV (cytomegaloovirus) may be a point for intervention. It is usually asymptomatic and a common virus in people and is known to have a powerful effect on increased immune aging. Similar to cold sores and shingles, CMV is mostly dormant but can occur when a person experiences high stress.
In the study, statistically controlling CMV positivity also decreased the link between accelerated immune aging and stress.
To view the original scientific study click below:
Social stressors associated with age-related T lymphocyte percentages in older US adults: Evidence from the US Health and Retirement Study



 Researchers have developed a new method called untargeted metabolomics that identifies the large number of molecules that come from our food. Most of these molecules appear in our blood and stool and had previously been unknown. This method can provide a direct way to detect hundreds of thousands of molecules that may now be used to make a diet profile of individuals and provide clues as to health outcomes.
Researchers have developed a new method called untargeted metabolomics that identifies the large number of molecules that come from our food. Most of these molecules appear in our blood and stool and had previously been unknown. This method can provide a direct way to detect hundreds of thousands of molecules that may now be used to make a diet profile of individuals and provide clues as to health outcomes. There are quite a few studies that indicate that cutting calories can improve the health of a person and enhance longevity. However, new research indicates an even greater effect when you play to your daily rhythm of eating only during times where there are highest levels of energy requirements in order to optimize longevity!
There are quite a few studies that indicate that cutting calories can improve the health of a person and enhance longevity. However, new research indicates an even greater effect when you play to your daily rhythm of eating only during times where there are highest levels of energy requirements in order to optimize longevity! Dementia is a life altering disease and affects millions of people and their families worldwide negatively. But in a new study, researchers have found a modifiable factor that could possibly lower the risk of the advancement of this condition before it becomes irreversible. Their work highlights the link between muscle mass and rapid cognitive decline.
Dementia is a life altering disease and affects millions of people and their families worldwide negatively. But in a new study, researchers have found a modifiable factor that could possibly lower the risk of the advancement of this condition before it becomes irreversible. Their work highlights the link between muscle mass and rapid cognitive decline.  Exercise is a great way to keep fit and stay healthy but now a new study has determined that the time of day to exercise and get the best results are different for men and women. The research team at Skidmore College performed a study consisting of a 12-week exercise program. The participants were 27 women and 20 men ranging in age from 25-55 years old. Because of this large number, they were split into workout groups in the morning and evening.
Exercise is a great way to keep fit and stay healthy but now a new study has determined that the time of day to exercise and get the best results are different for men and women. The research team at Skidmore College performed a study consisting of a 12-week exercise program. The participants were 27 women and 20 men ranging in age from 25-55 years old. Because of this large number, they were split into workout groups in the morning and evening. While it has been known that eating avocados is good for you, there has now been a new study detailing how they can improve unhealthy cholesterol levels. This has been the most extensive and largest study to date on the overall effects of health by consuming avocados including the length of the study period and the large number of participants.
While it has been known that eating avocados is good for you, there has now been a new study detailing how they can improve unhealthy cholesterol levels. This has been the most extensive and largest study to date on the overall effects of health by consuming avocados including the length of the study period and the large number of participants.  Longevity research has commonly used a nematode worm called caenorhabditis elegans in studies. This is due to its genetic makeup being similar to humans and it has a relative short lifespan, usually 4 weeks or less. Earlier research to improve these worms lifespan resulted in various interesting outcomes by modifying their rapamycin and insulin signaling pathways, which resulted in a 30% and 100% increase in their lifespan, respectively. The researchers then wondered what would happen from modifications made to both of these pathways at the same time.
Longevity research has commonly used a nematode worm called caenorhabditis elegans in studies. This is due to its genetic makeup being similar to humans and it has a relative short lifespan, usually 4 weeks or less. Earlier research to improve these worms lifespan resulted in various interesting outcomes by modifying their rapamycin and insulin signaling pathways, which resulted in a 30% and 100% increase in their lifespan, respectively. The researchers then wondered what would happen from modifications made to both of these pathways at the same time.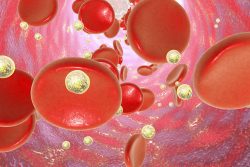 Bioengineers have discovered a new strategy that can restore stem cells that have been damaged and also enable them to grow new tissues again. The novel drug delivery system might help infants who were born from pregnancies that were complicated.
Bioengineers have discovered a new strategy that can restore stem cells that have been damaged and also enable them to grow new tissues again. The novel drug delivery system might help infants who were born from pregnancies that were complicated. By using a mouse model, researchers from the Univ. of Copenhagen have developed an alternative route for cells to follow to build organs. They used this information to attain a stem cell that is new and could possibly generate a supply of organs.
By using a mouse model, researchers from the Univ. of Copenhagen have developed an alternative route for cells to follow to build organs. They used this information to attain a stem cell that is new and could possibly generate a supply of organs.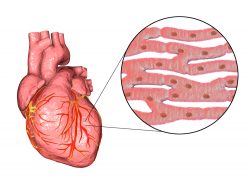 A team has reported new technology that will not only repair heart muscle cells in mice, but also can regenerate them after a heart attack. The groundbreaking discovery has the possibility to develop into an important clinical strategy to treat humans who have heart disease.
A team has reported new technology that will not only repair heart muscle cells in mice, but also can regenerate them after a heart attack. The groundbreaking discovery has the possibility to develop into an important clinical strategy to treat humans who have heart disease.