Relational Memory Benefits From Sleep
 While we sleep there are brain circuits and neuron learning connections that are active. They help us establish differences between items that are unrelated. The ability to remember indirect or arbitrary links between people, objects or events is called relational memory. This is what helps you put names with faces, find your keys or remember to turn off the stove before you leave the house.
While we sleep there are brain circuits and neuron learning connections that are active. They help us establish differences between items that are unrelated. The ability to remember indirect or arbitrary links between people, objects or events is called relational memory. This is what helps you put names with faces, find your keys or remember to turn off the stove before you leave the house.
It has been established that human and animal memory receives benefits from quality and sufficient sleep. New research is showing the hidden mechanisms that create or strengthen new relational memories while you sleep.
The researchers made an artificial model of 2 different areas of the brain. The cortical, which is involved in learning, memory and making decisions, and the thalamic, which has to do with prior sensory processing. The model simulated 2 major states of the brain. The first is awake, when the neurons are automatically optimized and active to generate sensory input. The second is deep sleep, when inherent oscillations of electrical activity is processed, such as waves that are slow.
The network model properties were able to be changed to generate transitions from asleep activity and awake activity comparable to brain activity every day.
In the region that is cortical, the neuron connections were able to become weaker or stronger dependent on their activity. This is called synaptic plasticity, and reflects the primary biological mechanism of the way memories are erased or formed.
The team modeled the cortex following visual processing, with one cortical layer which represented primary visual cortex and another layer which represented associative cortex. Each time one sees the exact object, the same neurons in the cortex that was visual was active. If someone sees two objects in the exact context, then these links might be learned in the cortex that is associative through strengthening connections between neurons that represent the two objects.
The team trained the network in the awake mode to determine direct links, such as A+B or B+C but not A+C, then found that in sleep, the model made indirect associations of A+C.
This occurred because during sleep the neurons which represented all three related items (A, B & C), automatically fired in close order that was temporal. This phenomenon is known as sleep replay and triggers synaptic plasticity and leads to the formation of powerful synaptic connections between all the neurons. This means that following sleep, activating any one of the groups such as A, activated all the other related groups – B and C.
The work is primarily conceptual, but the team states the work has implications that are real world. One that is important in the study is in informing studies of disease in the future – such as autism spectrum disorder and schizophrenia. Studies show that people who have these conditions do worse on relational memory tasks and also have sleep that is disrupted and that is slow wave.
The study has suggested the focus on improving sleep that is slow wave, which would alleviate some of the symptoms that are cognitive and associated with theses conditions, might be a more fruitful forward path rather than focusing exclusively on the cognitive symptoms.
The team notes that sleep quality and memory function do decline with the aging process, however current or even new technologies that augment sleep oscillations might help improve and protect functions of memory in the older population.
To view the original scientific study click below:
Role of Sleep in Formation of Relational Associative Memory



 As we age, we lose muscle mass and the risk of dementia, heart disease, and immune function decreases. As the years go by, it becomes more difficult for humans to rebound from injury, a workout or illness. Aging takes a big toll on muscle tissue. Scientists have discovered that one type of activity in particular puts this process in reverse.
As we age, we lose muscle mass and the risk of dementia, heart disease, and immune function decreases. As the years go by, it becomes more difficult for humans to rebound from injury, a workout or illness. Aging takes a big toll on muscle tissue. Scientists have discovered that one type of activity in particular puts this process in reverse.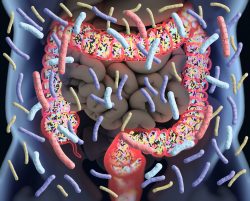 There are trillions of benign bacteria that live in our intestines. The immune system keeps them in constant balance which in turn ensures they are harmless to humans. A team has been able to demonstrate how some natural antibodies keep them in check. Their discoveries could make a substantial contribution to developing superior vaccines.
There are trillions of benign bacteria that live in our intestines. The immune system keeps them in constant balance which in turn ensures they are harmless to humans. A team has been able to demonstrate how some natural antibodies keep them in check. Their discoveries could make a substantial contribution to developing superior vaccines. A new study demonstrates that stress from things like job strain, traumatic events, discrimination, and everyday occurrences can accelerate immune system aging. This can possibly increase people’s chances of cardiovascular disease, cancer and illness due to infections. The study could offer an explanation in disparities in health that are age related which include the diverse toll of the COVID-19 pandemic and determine possible avenues for intervention.
A new study demonstrates that stress from things like job strain, traumatic events, discrimination, and everyday occurrences can accelerate immune system aging. This can possibly increase people’s chances of cardiovascular disease, cancer and illness due to infections. The study could offer an explanation in disparities in health that are age related which include the diverse toll of the COVID-19 pandemic and determine possible avenues for intervention. Researchers have developed a new method called untargeted metabolomics that identifies the large number of molecules that come from our food. Most of these molecules appear in our blood and stool and had previously been unknown. This method can provide a direct way to detect hundreds of thousands of molecules that may now be used to make a diet profile of individuals and provide clues as to health outcomes.
Researchers have developed a new method called untargeted metabolomics that identifies the large number of molecules that come from our food. Most of these molecules appear in our blood and stool and had previously been unknown. This method can provide a direct way to detect hundreds of thousands of molecules that may now be used to make a diet profile of individuals and provide clues as to health outcomes. There are quite a few studies that indicate that cutting calories can improve the health of a person and enhance longevity. However, new research indicates an even greater effect when you play to your daily rhythm of eating only during times where there are highest levels of energy requirements in order to optimize longevity!
There are quite a few studies that indicate that cutting calories can improve the health of a person and enhance longevity. However, new research indicates an even greater effect when you play to your daily rhythm of eating only during times where there are highest levels of energy requirements in order to optimize longevity! Dementia is a life altering disease and affects millions of people and their families worldwide negatively. But in a new study, researchers have found a modifiable factor that could possibly lower the risk of the advancement of this condition before it becomes irreversible. Their work highlights the link between muscle mass and rapid cognitive decline.
Dementia is a life altering disease and affects millions of people and their families worldwide negatively. But in a new study, researchers have found a modifiable factor that could possibly lower the risk of the advancement of this condition before it becomes irreversible. Their work highlights the link between muscle mass and rapid cognitive decline.  Exercise is a great way to keep fit and stay healthy but now a new study has determined that the time of day to exercise and get the best results are different for men and women. The research team at Skidmore College performed a study consisting of a 12-week exercise program. The participants were 27 women and 20 men ranging in age from 25-55 years old. Because of this large number, they were split into workout groups in the morning and evening.
Exercise is a great way to keep fit and stay healthy but now a new study has determined that the time of day to exercise and get the best results are different for men and women. The research team at Skidmore College performed a study consisting of a 12-week exercise program. The participants were 27 women and 20 men ranging in age from 25-55 years old. Because of this large number, they were split into workout groups in the morning and evening. While it has been known that eating avocados is good for you, there has now been a new study detailing how they can improve unhealthy cholesterol levels. This has been the most extensive and largest study to date on the overall effects of health by consuming avocados including the length of the study period and the large number of participants.
While it has been known that eating avocados is good for you, there has now been a new study detailing how they can improve unhealthy cholesterol levels. This has been the most extensive and largest study to date on the overall effects of health by consuming avocados including the length of the study period and the large number of participants.  Longevity research has commonly used a nematode worm called caenorhabditis elegans in studies. This is due to its genetic makeup being similar to humans and it has a relative short lifespan, usually 4 weeks or less. Earlier research to improve these worms lifespan resulted in various interesting outcomes by modifying their rapamycin and insulin signaling pathways, which resulted in a 30% and 100% increase in their lifespan, respectively. The researchers then wondered what would happen from modifications made to both of these pathways at the same time.
Longevity research has commonly used a nematode worm called caenorhabditis elegans in studies. This is due to its genetic makeup being similar to humans and it has a relative short lifespan, usually 4 weeks or less. Earlier research to improve these worms lifespan resulted in various interesting outcomes by modifying their rapamycin and insulin signaling pathways, which resulted in a 30% and 100% increase in their lifespan, respectively. The researchers then wondered what would happen from modifications made to both of these pathways at the same time.