Enhance Cognitive Youth with Online Brain Games
 A new study conducted at the University of California, Irvine, has found that online brain game exercises can help people in their 70’s and 80’s multitask cognitively even as well as people 50 years younger! This valuable tool, gives older adults the ability to handle today’s daily onslaught of information which can be very taxing for seniors.
A new study conducted at the University of California, Irvine, has found that online brain game exercises can help people in their 70’s and 80’s multitask cognitively even as well as people 50 years younger! This valuable tool, gives older adults the ability to handle today’s daily onslaught of information which can be very taxing for seniors.
Like our bodies, we can work out and train our brains to improve mental performance. The research has discovered that older people who completed some very specific tasks gained the ability to beef up their brain’s ability to switch between tasks in a game which was at a level similar to 20 and 30 year people who were untrained.
The findings emphasize the cognitive cost of multitasking. Multitasking dilutes function through splitting focus. The findings indicate ways in which people throughout their lifespan can beat brain drain which can be brought on by the natural aging process and the increasingly crowded multimedia environment.
For the study the team partnered with Lumosity which is an online platform offering a variety of daily brain training games. They focused on data obtained from Lumonsity’s “Ebb and Flow” game which is a task switching games which challenges the ability of the brain to shift between cognitive processes interpreting movement and shapes.
Of the millions of individuals who played Ebb and Flow between 2012 and 2017, the team randomly sampled performance of approximately 1,000 users within two categories – those who ranged in age from 21 to 80 and had finished fewer than 60 sessions of training; and adults aged 71 to 80 who had logged a minimum of 1,000 sessions.
The research team found that the majority of the older and highly practiced players matched or exceeded the performance of the younger users who didn’t play the game very much. Any lead seniors however, significantly declined after the 21 to 30 year old participants completed at least 10 practice sessions.
Improved lifestyles and advances in the medical field have allowed people to live longer. Brain health is an important factor in that equation. With consistent upkeep, cognitive youth can be retained into the golden years.
To view the original scientific study click below
A large-scale analysis of task switching practice effects across the lifespan.



 According to a recent study, 20 years of a sedentary lifestyle is linked to two times the risk of premature death when compared to being physically active. The HUNT study’s findings suggest that in order to get maximum health benefits from physical activity to protect against premature cardiovascular and all cause death, a person needs to be continually physically active.
According to a recent study, 20 years of a sedentary lifestyle is linked to two times the risk of premature death when compared to being physically active. The HUNT study’s findings suggest that in order to get maximum health benefits from physical activity to protect against premature cardiovascular and all cause death, a person needs to be continually physically active. A research team at the Osaka University has conducted the world’s first corneal tissue transplant using reprogrammed stem cells derived from skin tissue. The patient was a Japanese woman in her 40’s who suffered from an epithelial stem cell deficiency in her cornea. This condition can make vision blurry and can lead to blindness.
A research team at the Osaka University has conducted the world’s first corneal tissue transplant using reprogrammed stem cells derived from skin tissue. The patient was a Japanese woman in her 40’s who suffered from an epithelial stem cell deficiency in her cornea. This condition can make vision blurry and can lead to blindness. New research suggests that an upbeat view towards life might increase your odds for longevity. The findings come from a study looking at optimism and longevity among nearly 1,400 men and 70,000 women. The current study builds on previous research which linked higher levels of an optimistic view to reduced risks of premature death and chronic illness.
New research suggests that an upbeat view towards life might increase your odds for longevity. The findings come from a study looking at optimism and longevity among nearly 1,400 men and 70,000 women. The current study builds on previous research which linked higher levels of an optimistic view to reduced risks of premature death and chronic illness. A new study has shown that self administered acupressure can improve fatigue and pain symptoms in people who experience chronic lower back pain. This traditional Chinese medicine technique may be a better treatment than medication which can have serious side effects and can lead to addiction and abuse.
A new study has shown that self administered acupressure can improve fatigue and pain symptoms in people who experience chronic lower back pain. This traditional Chinese medicine technique may be a better treatment than medication which can have serious side effects and can lead to addiction and abuse. Adding Matcha Green Tea to your daily diet may improve your health and also help reduce anxiety. Experiments have shown that Matcha Tea’s anxiolytic effects happen because of the activation of dopamine D1 receptors and other serotonin receptors.
Adding Matcha Green Tea to your daily diet may improve your health and also help reduce anxiety. Experiments have shown that Matcha Tea’s anxiolytic effects happen because of the activation of dopamine D1 receptors and other serotonin receptors.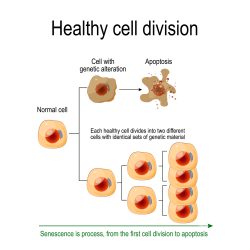

 A research team at the University of Illinois, Chicago and the University of Pennsylvania have developed a new and unique technique which uses flexible implantable bone stabilizing plates and stem cells to speed healing of bone defects or large breaks.
A research team at the University of Illinois, Chicago and the University of Pennsylvania have developed a new and unique technique which uses flexible implantable bone stabilizing plates and stem cells to speed healing of bone defects or large breaks.