Making Blood Stem Cells Young Again
Our blood stem cells generate around a thousand billion new blood cells every day. But the blood stem cells’ capacity to produce blood declines as we age. This leads to lowered immunity and other age related problems. Now for the first time, a research team at Lund University in Sweden has succeeded in rejuvenating blood stem cells that had become less functional in aging mice. The study is published in Nature Communications.
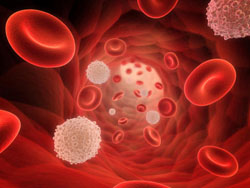
When we are young, our blood stem cells produce an even and well-balanced number of red and white blood cells according to need. As we age, however, the capacity of the blood stem cells to produce the number of blood cells we need declines.
“This type of age-related change can have major consequences as it can lead to an imbalance in stem cell production. For example, a reduced production of immune cells or excessive production of other types of cells” explains David Bryder, who headed the study at Lund University.
A fundamental question was whether blood stem cells age differently within a single individual or whether all blood stem cells are equally affected by advancing age. In an initial stage, it was therefore important to genetically mark old blood stem cells, to enable the identification and tracking of those most affected by age. In the next step, these traceable cells were reprogrammed to another type of stem cell known as iPS cells, which can generate all cells in an individual and not only blood cells. When the cells are reprogrammed, their identity is ?re-set”; when these reprogrammed iPS cells formed new blood stem cells, the researchers observed that the re-set had entailed a rejuvenation of the cells.
“We found that there was no difference in blood-generating capacity when we compared the reprogrammed blood stem cells with healthy blood stem cells from a young mouse. This is, as far as we know, the first time someone has directly succeeded in proving that it is possible to recreate the function of young stem cells from a functionally old cell?, says Martin Wahlestedt, the first author of the study.
The research team’s studies have also thereby shown that many age-related changes in the blood system cannot be explained by mutations in the cells’ DNA. If the changes depended on permanent damage at the DNA level, the damage would still be present after the re-set. Instead, epigenetic changes appear to underlie the decline in function associated with advancing age.
“Our findings justify further research to improve the function of human blood stem cells” concludes David Bryder.
Reference: Martin Wahlestedt, Eva Erlandsson, Trine Kristiansen, Rong Lu, Cord Brakebusch, Irving L. Weissman, Joan Yuan, Javier Martin-Gonzalez, David Bryder. Clonal reversal of ageing-associated stem cell lineage bias via a pluripotent intermediate. Nature Communications, 2017; 8: 14533 DOI: 10.1038/ncomms14533